PAEDIATRIC (CHILD) AND PREVENTIVE DENTISTRY (PAEDODONTICS)
What is paediatric dentistry (paedodontics)?
Paedodontics or paediatric dentistry is a branch of dentistry dealing with children, from their birth through adolescence. The main objective of paediatric dentistry is the prevention of tooth decay of primary (baby) teeth as well as the first permanent teeth.
What is the best time for Your child’s first dental visit?
According to the World Dental Federation, the best time for the child’s first dental visit is at the age of one, no later than the age three. During that first visit to our office, we will let you get acclimated and we will spend some time getting to know each other. This visit is also very important in order to educate the parents on the importance of baby teeth and prevention of early tooth decay, the significance of oral hygiene, the importance of a well-balanced nutrition and how to adopt healthy habits early on in life. It is desirable for the visits to occur every six months in order to gain the child’s trust, for the child to get familiarized with the staff, the office, the instruments and teeth in general, and with that, for the child to develop a positive attitude while feeling safe. These first check-ups, are also, incredibly important in order to diagnose a possible development of tooth decay, some undesirable habits and orthodontic anomalies. The teeth of our youngest patients, will be painted with a liquid, a gel or a varnish containing fluoride (fluoridation). This preventive treatment is completely painless for the child, whilst the fluoride helps to prevent tooth decay and strengthens the tooth enamel.
How to properly maintain oral hygiene in children?
Oral health of children begins by adopting proper habits of maintaining oral hygiene which children need to acquire early on and in that way prevent the occurrence of tooth decay in baby, and later on, in permanent teeth. Children should brush their teeth twice a day (until they are grown enough to maintain their hygiene by themselves, this should be done by a parent). The toothbrush should be adapted to the child, small and soft. In the beginning, during the eruption, teeth should be washed just with water, and later on, when the child learns how to spit the content from his/her mouth, you can start introducing toothpaste to your child. You have probably noticed that you can find specialized toothpastes adapted to a certain age of a child.While choosing a toothpaste, take notice of the fluoride level, making sure it is low (up to 500 ppmF), for children up to the age of six.Also, after brushing his/her teeth before bedtime, the child should avoid eating and drinking, especially having a bottle of sweetened liquids. This habit can cause baby bottle tooth decay – a dental cavity which attacks the front baby teeth destroying them completely up to their gums.We recommend you avoid giving your child sugary drinks altogether, or better yet, just give them water. Simple rules and habits which children acquire at their earliest age, are incredibly important for the rest of their life such as an adequate oral hygiene, a balanced nutrition and regular visits to the dentist. Through the age of four to five, the child is old enough to wash his/her teeth twice a day with the supervision and help from their parent. At the age of six, the child can use a toothpaste for adults (1000-1500 ppmF). At the age of seven, taking in account good coordination, the child should be able to brush his/her own teeth.
When do baby (primary) teeth come in and what is their total?
Primary (baby) teeth usually start coming in at the age of six months, and by the age of three, all of the 20 baby teeth should have erupted.
The importance of baby teeth
Baby teeth are very important because they allow proper chewing and promote normal development of the jaw bones, proper development of speech, development of the bite. But also because they act as placeholders for the permanent teeth and make sure they align properly through the course of their eruption.
If baby teeth are lost prematurely due to untreated tooth decay or trauma, the permanent teeth can’t erupt properly leading to the development of various orthodontic anomalies.
While they are erupting, permanent teeth break down the roots of their baby predecessors causing them to become loose and fall out, and in cases when they don’t fall out on their own, the child should be taken to the dentist to have the baby tooth removed.
In our office, after removing the tooth decay on baby teeth, we use a high quality aesthetic composite filling (fillings that match the colour of the tooth).
How does tooth decay occur in a child’s mouth?
The oral cavity of a child, right after birth, is free from bacteria, but at some point in life, bacteria start to inhabit the mouth and stay there through the course of the child’s life. Cariogenic bacteria can reach the child’s mouth while interacting with other children in kindergarten, and in the case of early tooth decay, bacteria is usually passed from the mother to the infant. These bacteria get passed on indirectly, through the saliva while the mother prepares the meal or feeds her baby. The mother uses the same utensil (for example, in order to taste the meal) and then uses the spoon to feed the baby and with that, bacteria from her mouth reach the babies mouth. Besides the contamination of the child’s mouth with cariogenic bacteria, early tooth decay in children, is also caused by a diet high in carbohydrates and an inadequate oral hygiene. When all of these factors are combined, an aggressive form of decay occurs (baby bottle tooth decay) which causes a significant damage to baby teeth.
What is baby bottle tooth decay?
Baby bottle tooth decay is an especially aggressive form of early childhood caries. It occurs in toddlers up to the age of three due to bad hygiene and frequent consumption of sweetened liquids through a baby bottle, in the evening before bedtime or throughout the day. The early aggressive childhood caries first appears on the outer parts of upper front (maxillary anterior) baby teeth, right near the gum line. Usually, the decay affects more teeth at once, and often it affects the entire upper teeth line. Quickly, the decay spreads to baby molars. If early baby decay is left untreated, very shortly it destroys the entire crown of upper baby teeth, leaving them to look like they have been aligned with the level of the gums.
Infection spreads into the pulp of these teeth which can lead to dental abscess and dental fistula. In such an advanced state of infection, it is necessary to perform an immediate treatment, sometimes with the usage of sedation or general anaesthesia.
On the opposite, with timely recognition and treatment of baby bottle decay and applying a preventive set of measures, it is possible to prevent such a major destruction of baby teeth, and to spare the child of great pain and a stressful dental treatment.
What are the consequences of baby bottle tooth decay?
The consequences of baby bottle tooth decay are associated with:
- Nutrition – destroyed baby teeth make proper chewing impossible which puts a burden on digestion and can slow down the overall growth of a child
- Speech – the loss of the front teeth can lead to unclear speaking patterns making it difficult for a child to properly pronounce certain letters like R,S,V,Z
- Pain – teeth destroyed by decay inflict pain, swelling, bleeding and bad breath, and the infection can damage the permanent tooth development
- Irregular positioning of permanent teeth can be caused by a premature loss of baby teeth which serve as placeholders for their permanent replacements (successors)
- Tongue thrusting into the empty space of the mouth can cause misalignment of newly erupted teeth outside the teeth line
- Psychological changes – a child can feel unease due to the imbalance of aesthetics or his/ her appearance which can lead to introversion or a hyper need to deflect attention from his/her teeth onto other attributes or can cause jealousy of their peers with a beautiful smile
How can baby bottle tooth decay be prevented?
This type of early baby decay or baby bottle tooth decay can be prevented in an efficient way, simply by following a few instructions:
In order to avoid the contamination of the babies mouth with cariogenic bacteria, it is necessary not to feed the baby with the same utensil being used by other people. It is, especially, important for the mother not to try out the food with the same spoon with whom she is feeding the baby. This is, usually, the most frequent way how bacteria get passed on to the baby which causes the early tooth decay.
Baby food is, often, rich with simple carbohydrates (sugars) which are known to cause decay. If intake of sugar can’t be avoided, it must be controlled. The most important thing for a parent is to thoroughly clean the babies’ teeth after the last meal and before bedtime and not to give them sweetened liquids during night time.
The most common and usual mistake a parent makes is putting the baby to bed with a sweet drink or giving them the drinks during the night. During sleep, the secretion of saliva reduces significantly and there is a lack of movement of cheeks and lips which ensure the self-cleaning of dental surfaces. With that, sugars grip the surface of teeth and with time make it possible for cariogenic bacteria to develop.
In order to avoid this, it is necessary to thoroughly clean the teeth with a toothbrush before bedtime (in infants, using a damp gauze or special cleaning wipes) and to give them only water during night. If the child, nevertheless, does consume food or sweet beverages, before going back to sleep, it is necessary to repeat the cleaning of teeth.
Using fluoride toothpaste and by professional fluoridation, the baby teeth enamel becomes stronger and less sensitive to the effect of bacterial acids. Therefore, it is important to schedule regular dental check-ups (at least every six months, if necessary more often) to ensure fluoridation of baby teeth and the education of parents on the proper measures of oral hygiene. Being regular with the check-ups is, also, important for early detection of baby decay and timely treatment.
What is mixed dentition stage?
The mixed dentition stage refers to the presence of deciduous (baby teeth) and permanent dentition (permanent teeth) in the oral cavity of a child. It lasts between the ages of six and twelve. At the age of twelve, the remaining milk teeth (second molars) are being replaced with their permanent successors (permanent premolars). This stage is followed by the period of permanent dentition. A completely developed permanent dentition consists of 32 teeth: eight incisors, four canines, eight premolars and twelve molars.
When does eruption of the first permanent teeth start and what is the chronology of eruption?
Eruption of the first permanent teeth, usually, starts at the age six. It begins with wobbling and shedding, firstly of the lower central incisors (first teeth from the centre of the mouth), but also with eruption of the first permanent molars (sixth teeth) which don’t have its milk predecessors. It is very important for parents to realize that the bigger molar which, usually, erupts at the age of six, and is located at the end of the teeth line, is in fact a permanent tooth. It is important for parents not to confuse these first molars with baby teeth and neglect in the case of decay. Protection of permanent molars with fissure sealant as soon as their crown erupts, is also an effective way of preventing decay of permanent teeth. As a rule, the first teeth to erupt are the ones in the lower jaw: permanent lower second teeth (lateral incisors) emerge between the ages of seven and eight, and upper between the ages of eight and nine. Permanent lower third teeth (canines) between the ages of nine and ten, and upper between the ages of eleven and twelve. Permanent lower fourth teeth (first premolars) between the ages of ten and twelve, and upper between the ages of ten and eleven. Permanent lower fifth teeth (second premolars) between the ages of eleven and thirteen, and upper between the ages of twelve and thirteen. Permanent lower seventh teeth (second molars) emerge between the ages of eleven and thirteen, and upper between the ages of twelve and thirteen. Permanent upper and lower eighth teeth (third molars, wisdom teeth) emerge between the ages of seventeen and 25. Milk fourth and fifth teeth (milk molars) remain for a fairly long time in the mouth, so it is necessary to pay special attention to them because these teeth are very important for the placement of their permanent successors. The period of eruption of permanent teeth differs from person to person, and there is always a possibility for either earlier or later emergence of certain teeth than what we know to expect from the chronology of emergence. However, in cases where one or more teeth aren’t emerging as they should be, it is necessary to seek advice from a dentist.
What if a permanent tooth isn’t emerging when it should be?
If a certain permanent tooth isn’t emerging when it should be, it is necessary to make an x-ray of the jaw (most commonly an orthopantomogram) to make sure the tooth is even present in the jaw, and if it is, whether its emergence is being blocked by an obstruction of some sort. (for example, a residue of a baby tooth, a bone, insufficient room in the dental line…). Teeth which usually don’t have their permanent successors (Anodontia) are the upper second teeth, premolars and wisdom teeth. It is common for an impacted or an unerupted tooth to remain behind in the bone of the jaw line. Besides the wisdom teeth, any other tooth can become impacted or unerupted, but this usually occurs in the maxillary cuspids and lower premolars.
What is fissure sealant (dental sealant)?
Fissure sealant is a preventive paedodontic procedure used in order to protect the permanent teeth from decay development.
Due to the specific build of a dental crown, its specific reef with its deep fissures (grooves of narrow entrance and a wide bottom) and its pits, it is difficult to maintain a proper hygiene in children.
This results in plaque accumulation in the fissures which result in decay development. More than 75 % of decay begins in those deep fissures. Incidence of decay in the fissures is the highest in the first four years after the emergence of permanent teeth. The procedure itself, of placing fillings or fissure sealants is completely painless. The fissures of the tooth are cleaned (without drilling) and are filled (etched) with an aesthetic composite material which matches the colour of the tooth.
Such a deep fissure of a tooth becomes shallow and accessible for cleaning. It is recommended to perform the procedure, prior to the emergence of the dental crown of the first permanent molar (sixth, which emerges around the age of six) when the presence of cariogenic bacteria in the fissures isn’t at its highest.
Fissure sealant can also be used for protection of other molars (the seventh teeth) around the age of twelve, and premolars (the fourth and fifth teeth), as well as baby teeth.
By all means, it is essential to implement a proper oral hygiene and to keep up with regular cheek-ups with the dentist for the fissure sealants to be controlled or perhaps replaced if necessary, and with that to avoid a possible development of decay.
How does dental trauma occur?
Dental trauma occurs by a short aggressive force which leads to tearing of the hard dental tissues.
Fractures can occur directly (with a direct hit to the teeth) or indirectly (by a hit to the lower jaw in which the lower teeth collide with the upper ones at great speed). Trauma mostly impacts the front teeth of both jaws, while trauma of the back teeth is quite rare. Dental trauma occurs mostly in pre-schoolers and adolescents, and is most often present in car accidents and contact sports.
Damages of the hard dental tissue can differ in range – from an insignificant and, almost, an unnoticeable tear (crack) of the enamel, up to the fractures of the larger part of dental crowns.
Types of dental trauma:
Dental trauma can be:
- an infraction – the smallest fracture without the loss of tooth structure. The enamel is slightly cracked, but not detached from the rest of the dental crown. At the place of infraction, a crack that varies in colour and transparency from the surrounding enamel, is noticeable. The crack is best seen when the tooth is directly lit up, even though in daylight it is not noticeable. This condition doesn’t cause any disturbances and treatment is not necessary
- an enamel fracture – occurs due to a chipped fragment of dental surface and when there is a visible defect of the hard dental tissue. The fractured fragment can differ in size, and is sometimes so small that the fracture is barely visible. At the place of fracture, the enamel surface is rough and can at times cause a mild discomfort when touched by the tongue or with lips. Seeing how there is only damage to the enamel, there is no dentin harm (no visible sign of exposed dentin) or painful sensitivity. There can be some insignificant sensitivity to cold or hot stimulus because of the diminished thickness of the enamel surface which serves as a heat insulator of the dentin. If the patient finds and keeps the fractured enamel fragment, the defect is possible to repair by bonding it to the tooth. If the fragment isn’t available, the defect can be fixed using composite resin which replaces the lost part of enamel.
- an enamel and dentin fracture – besides the outer surface of the tooth (enamel), the trauma can also cause damage to the deeper tooth layer (dentin). When this layer is exposed to the workings of oral cavity, pain as well as sensitivity to hot, cold and sweet stimulus develops (occurs). Painful sensitivity depends on the damage range and the surface of the exposed dentin. The bigger the fractured fragment of dentin, the bigger (sharper) the pain. Same as with the fractured enamel, the defect can be repaired by bonding a fragment or with composite resin. If there is great damage, the tooth can be covered with an aesthetic veneer or a dental crown. In any case, by closing the damage in the dentin, pain and hypersensibility will subside.
- an enamel and dentin fracture with an exposed pulp – when the fracture line goes deeper into the tooth, opening of the pulp chamber can occur. (the space inside the tooth where the soft tissue of the tooth resides, including blood vessels and nerves). In that instance, there is bleeding from the pulp accompanied with pain and extreme sensitivity of the exposed pulp. It is not necessary for the damage of the hard dental tissue to be large in order for the pulp chamber to become exposed, it is enough just for the fractured fissure to be deep enough. On the other hand, the damage can be quite large and for the entire dental crown to be displaced. Irregardless of the damage range, the exposed pulp is susceptible to inflammation and necrosis and there is no way of preserving it. In that case, an endodontic procedure is being performed which includes removal of the pulp, cleaning and shaping the root canals as well, as filling them. Then, the crown defect gets restored with a filling or with a fixed prosthesis. Very often, due to the gravity of the defect, it is necessary to build a base over which a dental crown is being placed.
- with the narrow crown and root fractures of teeth, treatment is quite complicated due to the large defects of the hard dental tissue. The fractured fissure starts on the top of the crown, goes sideways near the root and ends on the top of the root which is located underneath the alveolar bone. Treatment of the defect is demanding because it requires the reconstruction of the tooth fragment located underneath the bone level. Treatment involves removal of the fractured segment, that is, an endodontic therapy, and the crown-root defect gets repaired by placing an implant crown. At times, due to the adverse positioning of segments, reconstruction is impossible and extraction is inevitable.
- a root fracture – the fracture is in oblique plane across the root, and the fracture is, entirely, situated below the bone line. During the medical examination, damage to the tooth isn’t visible, but pain when biting and increase in the mobility of tooth, suggest otherwise. Clinical findings of this sort of trauma, require an x-ray in order for the fractured segment to be seen. Treatment is fairly simple, and it involves immobilizing (preventing the movement) of the damaged tooth. The tooth is stabilized with a flexible splint for the adjacent teeth, so it doesn’t move with chewing. That enables the fractured root segments to grow back together. During the immobilization, it is advised to avoid chewing with the damaged tooth to minimise the movements which could slow down the recovery. After the fusion of segments, an endodontic procedure is necessary seeing how the trauma causes pulp necrosis.
Besides the trauma of dental tissue, there is also the trauma of its supportive tissues (periodontium).
Types of supportive tissue trauma, how do they occur and how are they treated?
Trauma of supportive tissue (periodontium) can occur due to a direct or an indirect hit to the tooth. Depending on the amount of force causing the trauma, they can either be mild and simple to treat, or very grave so salvation of the tooth becomes questionable.
There is the:
- concussion or contusion of the tooth; a mild damage of the periodontium caused by a mild force. Tooth is not displaced, there is no visible bleeding, and there is only a slight sensitivity while biting. There is, usually, no treatment necessary, and the periodontium should recuperate in a couple of days. Chewing with the damaged tooth should be avoided, and if greater pain occurs, the tooth can be immobilised with a dental splint.
- subluxation – caused by a force so powerful to tear some of the periodontal ligament fibres in charge of keeping the tooth in place in the alveola. The rest of the intact ligaments keep the tooth in place, so there is no displacement. But there is the presence of increased mobility that can be of various degree – from a mild up to a severe mobility. Due to the damage of periodontal blood vessels, around the edge of the dental crown, bleeding can appear. Pain is present by putting pressure and with movement of the tooth. Treatment involves placing an immobilizing splint for a week. The splint is mostly maid out of thin wiring which is “glued“ by a composite material to the damaged tooth and adjacent teeth. The split stabilizes the tooth and prevents displacement which can cause pain and slow down the healing. If the subluxation isn’t major, it is sufficient just to avoid chewing with the damaged tooth which will remove the need for splinting.
- luxation – a stronger impact causes a major damage to periodontal ligaments and the tooth becomes displaced from its usual spot. Depending on direction of the impact, the tooth can be pushed aside (lateral luxation), partially displaced out of the socket which makes it seem as if it is too elongated (extrusive luxation) or it is imprinted into the alveolar bone making it seem not emerged enough (intrusive luxation). In all of these cases, there is a presence of greater periodontal ligament damage manifesting in bleeding around the tooth crown, and there is also sensibility to pressure and mobility of the tooth. However, the tooth doesn’t have to be mobile – if the trauma leaves the tooth imprinted into the bone (like with the intrusive and some lateral luxations), then the neighbouring bone keeps it firm (steady) and doesn’t allow movement. In that case, the loosening of the tooth isn’t visible, even though the displacement of the tooth is obvious and trauma of periodontium is quite substantial. On the other hand, with extrusive luxation, the tooth is moved peripherally from the alveolar bone so the displacement is very revealed. Luxation treatment involves repositioning and immobilisation of the tooth. Reposition refers to re-inserting the displaced tooth into its original location, after which it is stabilized with a splint. Splint is usually worn in a period of seven – fourteen days, depending on the gravity of trauma. After the splint treatment is finished, periodontal ligament is, almost, completely regenerated, and the looseness and sensitivity to pressure disappears. After a couple of months, post to treatment, it is necessary to examine the pulp vitality. Trauma causing a significant displacement of the tooth, also results in damage of blood vessels which pass the tooth through the apical foramen. Damage to these vessels cut the blood circulation to the pulp which results in pulp necrosis. In cases of greater teeth displacement, there is a greater damage of blood vessels so pulp necrosis is more likely to happen. Signs of necrosis often go without noticing, immediately after trauma, and can be put off for a couple of months. This stresses the importance of pulp vitality examination, as well as an endodontic treatment in case the necrosis is determined.
- avulsion (knocked out tooth) – knocked out tooth is the hardest injury of the supportive apparatus inflicted (caused) by a high force magnitude. The tooth is completely displaced out of socket, accompanied by lots of bleeding. The injury seems a lot worse than it actually is – blood gets mixed with saliva, making it seem like the bleeding is quite more massive, and the accompanied damages of the soft tissues and the bleeding, give the impression of a great trauma. Seeing how it is most common in children, the trauma often causes panic with the injured person, as well as with the person witnessing the trauma. Despite of the dramatic appearance, this is not the case of a large injury, and with the timely intervention, it is possible to save the damaged tooth. The most important thing is to keep the knocked out tooth in a storage media, and contact a dentist as soon as possible who will proceed with treatment. Depending on the circumstances of the place of accident and available means, the tooth can be kept in different media:
- a) Dental alveolus (tooth socket)– the biggest chance for a knocked out tooth to be salvaged is for it to be replanted immediately straight back into the socket. The tooth has to be clean (it can’t be contaminated with soil, dust or other debris), and the alveolus mustn’t be damaged. The tooth should be rinsed quickly using cold water and replanted into the bloody alveolus, avoiding the use of pressure. A piece of tissue or a gaze is placed over the tooth which the patient softly bites on and with that holds the tooth in place until seeing a dentist. Even though, this is the best way to keep a damaged tooth, it is the least applied one. Due to fear and the dramatic look of the injury, the patient and other people caught on the scene of the accident, avoid tampering with the injury and putting the tooth back in place.
- b) Saliva – keeping the tooth in one’s own saliva is also, a good solution, until seeing the dentist. The tooth can be kept in a glass filled with saliva, and even a simpler way is for the tooth to be kept inside the oral cavity. The knocked out tooth is placed in the vestibule of oral cavity (between lips and teeth) and held in place with lips. In so, no unknown material or dirt can be present in the mouth, as well as bleeding. The lack of this approach is the danger of aspiration (inhalation) of the tooth which can cause suffocation. So, it is important for the injured person to stay calm and collected during the storage of tooth in the mouth. This is rarely the case with children, and they are the ones mostly inflicted to the avulsion of teeth and so keeping the tooth in their saliva is also, rarely applied.
- c) Milk – an extremely viable storage media for keeping the tooth and fairly accessible. Due to the simple handling and availability, milk is the best option for storing the avulsed tooth. The tooth should be briefly rinsed under cold running water and kept in milk until seeking dental treatment. The root surface mustn’t be scrubbed or irrigated with alcohol or other type of disinfectant.
Other storage media (regular water, alcohol, dry tissue) isn’t suitable for keeping the knocked-out tooth, but is used, most, often. In fact, the success of replantation depends on the vitality of periodontal ligament cells remaining on the surface of the knocked out tooth. Those cells need to maintain their vitality while the tooth is outside of its socket. The best chance for survival, have teeth which are replanted immediately after the avulsion, into their original environment, the tooth socket.Storing the tooth in saliva or milk is a good alternative, and other media should be avoided because they damage the periodontal ligament cells and minimise the success of replantation. Sadly, these other media are what is mostly being used because they are easily found on the scene of the accident and seem as an obvious choice to people aiding the patient. Besides the storage media, for a successful replantation, time plays the key role. The longer the tooth resides outside the socket, replantation has smaller odds for success, due to crashing of periodontal ligament cells. By keeping the tooth in a proper storage media, those cells can be kept alive and intact. By keeping the tooth in milk, cells can survive for around six hours. That time is sufficient to contact a dentist and for replantation. There are some professional storage media where the tooth can be kept up to several days, but they are rarely available at the scene of the accident. The treatment for dental avulsion is replantation. After visiting the dental office, the dentist immediately replants the tooth into a previously cleaned and prepared tooth socket. The tooth is stabilized using a splint which is to be worn for 14 days. Seeing how there is a disconnection of blood vessels supplying the pulp, the pulp atrophies and an endodontic treatment is needed. It is performed after the tooth has been stabilized into the socket, mostly after the two weeks, that is, right before removing the splint. Prognosis of the replanted tooth, is strictly dependent on the time the tooth spent outside the socket and the storage media. Replantation is not an option, if the tooth wasn’t kept in a proper storage media or has spent too much time outside the socket. In that case, the cells on the root surface have atrophied which makes coalescence with the periodontal tissue, impossible. That kind of tooth, wouldn’t be able to regenerate the periodontium, it would coalesce with the bone and resorption of its root would occur, which would result in the loss of the tooth.
How to protect the children’s teeth while playing sports?
For children, who are more susceptible to teeth trauma, because of the sports they partake in (especially contact sports, such as hockey, karate) it is recommended to wear personalized mouth protectors (mouth guards). We make such personalized sport guards in our dental laboratory based on the imprint taken in our office.
Unlike the regular protectors bought at a store, the personalized (customized) guards don’t create problems with breathing or talking, don’t fall out of the mouth so the children can focus on their sport activity. Dental protectors (protective guards) can be made in different colour, even with different writing, depending on the wish of the athlete, and the only condition is for all the teeth to be treated. With that it is important to stress that just one tooth is more important than the most expensive protective guard.
When is the best time for the first orthodontic visit?
It is recommended that the first orthodontic visit should be somewhere around the age of 6 or 7, when first permanent teeth appear. Based on the clinical examination and orthopantomogram (a panoramic X-ray of jawline) the orthodontist will determine the relation between primary and permanent teeth, whether all permanent teeth buds are present, if the upper and lower jaw relationship is favourable, whether there are any unfavourable habits (tongue thrusting, finger sucking, mouth breathing, etc.) and will advise parents on whether the treatment is necessary. If it is, the orthodontist will determine the best time to start the treatment in order to avoid wearing braces for too long unnecessarily. In any case, with early prevention and treatment, any irregularities of the jawline and teeth, can be corrected in a quick and successful manner.
What is the dental treatment procedure for children?
- After a high quality first exam and medical history taking (for which we need the parents’ cooperation when small children are in question) and a multidiscipline analysis of the state of children’s teeth, an optimal plan of treatment is determined as well as, giving advice on the proper oral hygiene of the child.
- All interventions in the oral cavity of a child, as well as repairs, we tend to perform in a completely painless manner, with the use of local anaesthetics intended for children thus avoiding the possibility for the children to have a bad experience. The procedure of giving an anaesthetic is also painless, we start with a spray anaesthetic which numbs the spot through which we will administrate the stronger injection anaesthetic. That way, even the prick of an injection goes without pain.
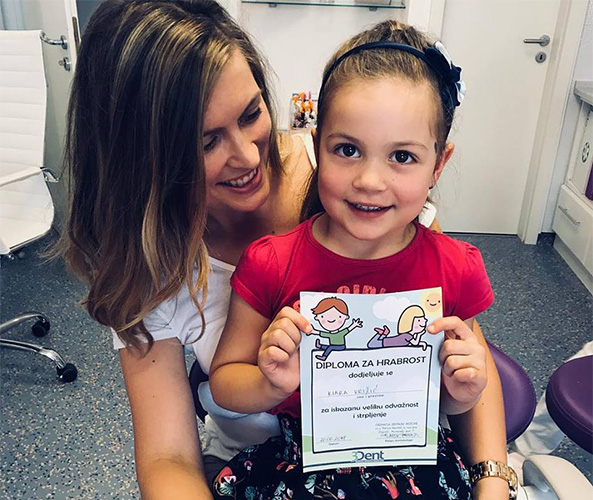
- Now, the tooth is being repaired. To make the fillings, used on permanent as well as baby teeth, we use an aesthetic composite filling that matches the colour of the tooth and aim to entirely mimic the morphological shape of the tooth in question. The fillings get polished. All small children brave enough to go through the treatment, get a special certificate for courage.
Why choose to entrust your child’s health to our professionals?
- We have 17 years of experience in paediatric and preventive dentistry.
- Each step of the treatment Your child is about to undergo will be explained to You, as well as all the other treatments and their advantages and risks.
- Each child is different so we first try to get to know them, adjusting our work to suit their individual needs and make them feel safe and comfortable.
- The work in Your child’s mouth will be painless and safe. Our practice is not a place where children feel pain, but rather a place where pain is prevented or terminated.
- All treatments will be performed with high-quality materials.
- At any moment we are available to you for advice and consultation via mobile phone, e-mail and social media.
- We try to keep our appointments.
- You can pay in cash, but also in interest free instalments: American Express up to 12 instalments, Diners up to 6 instalments, Erste & Steiermärkische bank Maestro and MasterCard up to 12 instalments.
- There is free parking in front of the practice.
If you think we can meet your criteria, feel free to contact us and make your appointment.
If you’re unable to find an answer to your question about paediatric dentistry, dental health or dental services, please feel free to contact us.
We are at your disposal!
| Radno vrijeme
PON, SRI, PET 9:00-16:00
UTO, ČET 13:30-20:30
☎ +385(0)1 4822 137






